The British Psychological Society publishes a Research Digest, and the latest one lists:
10 of The Most Widely Believed Myths in Psychology
http://digest.bps.org.uk/2016/07/10-of-most-widely-believed-myths-in.html
Here is Myth No 3:
3. Violent offenders usually have a diagnosis of mental illness
When people with mental health problems commit violent crimes, the media takes a disproportionate interest. No wonder that surveys show that most of the public believe that people with mental illness are inherently violent. In fact, as Scott Lilienfeld and his colleagues explain in the 50 Great Myths of Popular Psychology, the evidence suggests that at least 90 per cent of people with mental illness do not commit violent acts, and the overwhelming majority of violent offenders are not mentally ill. Some patients with specific conditions (such as command-based hallucinations "telling them" to commit acts) are at increased risk, but actual acts of violence are rare. A telling meta-analysis from 2011 concluded that 35,000 high-risk patients with a diagnosis of schizophrenia would need to be permanently watched or incarcerated to prevent one killing of a stranger by a patient.
In my last post I looked at the relevant item written by Scott Lilienfeld and colleagues in 50 Great Myths of Popular Psychology and found that the first few references, in my view, were not the endorsements that Lilienfeld and colleagues imagined they were, and that they had not dealt with the proper epidemiological papers in sufficient detail. (He disagrees, and will be writing a reply in due course). I thought that the rough estimate of male schizophrenic patients being five times more violent than members of the public was probably right.
Looking back at the BPS Research Digest I realized that I had not dealt with the last claim made in that publication, that “35,000 high risk patients with a diagnosis of schizophrenia would need to be permanently watched or incarcerated to prevent one killing of a stranger by a patient.” Here is the relevant paper:
The Predictive Value of Risk Categorization in Schizophrenia
Matthew M. Large, Christopher J. Ryan, Swaran P. Singh, Michael B. Paton, and Olav B. Nielssen,
(HARVARD REVIEW OF PSYCHIATRY 2011;19:25–33.)
DOI: 10.3109/10673229.2011.549770
You might imagine from the BPS Research Digest that this paper shows that you cannot detect which schizophrenic patients will be violent. Not really. The paper discusses whether a screening test applied to all schizophrenic patients would be able to detect a series of harms which vary considerably in frequency. The least frequent is the killing of a stranger in any one year, and that provides the astounding “35,000 patients to prevent one death” headline. Other harms are much more frequent, and more easy to detect. In defence of the above authors, their calculations are based on two assumptions: that the actuarial risks they use are the correct ones, and that the screening methods deployed are the best available. There are also new findings, available since they wrote their paper, to which I refer at the end of the post.
The base rates used by Large and colleagues are annual risk figures, not risks for longer periods. They derived them from from the published literature up till 2010.
As to screening instruments, Large et al mention Psychopathy Checklist–Revised (a semi-structured interview and questionnaire to elicit psychopathic personality); Historical Clinical Risk Management (specifically assessing violence risk from a historical, current and future perspective); Manchester Self-Harm Rule (assessing self harm and suicide risk), and the SAD PERSONS scale (suicide risk). So only the second scale is directly concerned with estimating the risk of violence to others. It is a well-validated scale with an extensive bibliography.
Is it any good at predicting violence? In a reassuring move, they answer this question using Receiver Operating Characteristics statistics, which show the overall accuracy of the measurement approach. I first came across this concept in the papers on attention written by John Morton, who thus taught me about ROCs and d prime long ago. Thanks, John.
A given area represents the probability that a randomly chosen person who scores positive on the dependent measure (in this study, is actually violent) will fall above any given cut-off on the predictor measure, and that an actually non-violent person will score below the cut-off (Mossman & Somoza, 1991). Thus, an area of .75 means that there is a 75% chance that an actually violent person would score above the cut-off for violence on the predictor, and an actually non-violent person would score below the cut-off. AUC values of 0.70 may be considered moderate to large, and .75 and above may be considered large.
The reported AUC values are in the .60s, .70s and some .80s according to which samples are being studied. In fact, the instrument is a good approach, and worthy of being improved further.
Rather than screening methods, I think that Operational Research is better. For example, evaluate those patients with prior problems of violence when they request re-admission for treatment (since not all those who apply can be admitted for treatment). That group will have a higher probability of offending than patients who comply with their medication. An illustration of the possibilities for a Bayesian approach can be derived from the very tables of frequencies given by the authors below.
The Large et al. paper is a careful piece of work, and I like their general approach. They know that actuarial methods are better than clinical judgment. They create a hypothetical screening instrument, but admit that the base rates for different harms are very different, and decide to use the same cut-offs for all harms, which may reduce the detection of violence to others. ROC curves would have been a welcome addition for comparative purposes. However, they say that they have set sensitivity and specificity to 80% each, exceeding what is reported in the general literature for future violence.
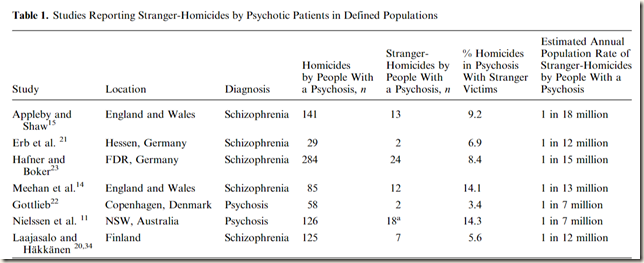
Here is the crucial table:
As you can see, assaults are committed by 1 in 7 untreated schizophrenics and by 1 in 10 treated schizophrenic patients per year. Treatment is only moderately effective in this regard. These are very high rates compared to the general public. Even with a relatively weak predictor, you need to monitor only 2 or 3 patients to possibly prevent an assault. This would be a highly effective intervention, and should receive more publicity. Large et al. seem to be doubtful about the value of screening in general, but their own data show it has utility for assaults.
For violent crime, monitoring 26 patients is required for a possible prevention of a violent crime. Again, this is manageable given resources.
Homicide in untreated patients happens, according to this table, at the very high rate of 1 in 600 schizophrenics. That compares with homicide rates in the UK of 0.9 per 100,000 persons and in the US of 3.9 per 100,000 persons. (US 4 times as murderous as the UK). So, the rate of homicide in non-schizophrenics in the UK is 1 in 111,111 and in the US is 1 in 25,641 persons. Therefore, an untreated schizophrenic person, using the estimates given in this paper, is apparently about 42 times more likely to murder someone than a US citizen, and 185 times more likely to murder someone than a UK citizen. Can these figures be correct? If so, this is a very dangerous category of person. An instrument with a positive predictive value of 0.66% (extremely low) requires that 151 persons be monitored. This would be onerous, but would prevent a murder. It is an indicator of the level of risk to the population when patients do not take their medication.
A homicide committed by a treated patient (1 in 10,000) means that treated schizophrenics are apparently 11 times more dangerous than UK citizens and almost 4 times more dangerous than US citizens. In the US it requires 2500 patients being monitored, a high number, and the best estimate of how difficult it would be to prevent one person being murdered, assuming most patients comply with treatment. Monitoring for most patients would probably involve no more than chasing up non-attenders at follow-ups, and doing some random checks on compliance with medication. This would be worth studying, particularly now that monitoring in diabetes is being trialled using mobile phone apps, with good results.
Here are a few reflections. Risk estimates vary considerably, but all are raised for schizophrenics, particularly in the early untreated phase. By implication, a schizophrenic patient who does not comply with medication falls into a high risk category. It seems very worth-while to screen for assaults, violent crime and homicide, particularly in untreated or medication-refusing schizophrenics.
Being alarmed about schizophrenia is understandable, and wishing them to have treatment and comply with treatment is also comprehensible. Screening schizophrenic patients in the UK is even more valuable than in the US, because of the massively increased risks compared to the lower UK norms.
Please check all these above figures for me. I have difficulty believing these risk estimates because they are so high. Clearly, detection rates are poor when the base rates are low, a familiar problem in signal detection of all sorts. The BPS Research Digest headline of the rarity of a schizophrenic committing a “stranger murder” is somewhat misleading, because we do not immediately have an accessible figure for “stranger murder” committed by the general public. One has to go through Bureaux of Justice Statistics 2008 to find that 25.5% of male murder victims and 11.9% of female murder victims are murdered by a stranger. Since 90% of offenders are male, I would guess that stranger murders are about 24% of the US total. Thus, in the US context, a US schizophrenic murders strangers at the rate of 1 in 140,000 and a normal US citizen murders strangers at the rate of (1 in 106,838) if I have done the sums correctly. Something wrong, I suspect. I looked up the original reference for this estimate, from Nielssen et al 2009, who is also co-author of the main paper being considered here.
Neilssen et al. say: A fixed effects model was used to calculate a pooled proportion of stranger homicides of 9.0% of all homicides by people with psychosis.
A fixed effects model was therefore used to calculate a pooled rate of stranger homicides committed by offenders with psychosis of 1 in 14.3 million people per year (95% CI=1 in 18.9 million per year to 1 in 11.5 million per year, Z=8.278,P<0.001). If it is assumed that 0.5% of the population have schizophrenia, the annual risk of a stranger homicide by a person with schizophrenia can be estimated to be about 1 in 70 000 patients per annum. If the prevalence of schizophrenia-related psychosis is assumed to be 1%, the estimated risk of stranger homicide is lower, about 1 in 140 000 patients per annum.
This explains the estimate used in the 2011 detection paper. However, if events have been under-recorded in the published literature, then the rates could be somewhat higher. I see the rates as quite variable, typical of rare events. However (see Sariaslan et al. paper below) the meth0ds do not give us certainty that all instances have been captured. At this stage I will need to do further work to understand the “stranger murder” calculations.
Here is a more recent finding about the general dangerousness of schizophrenia in a full population sample of 3,232,010 from Sariaslan, Larsson and Fazel (2015):

We observed that nearly one in four (23%) schizophrenia patients had ever been convicted of a violent crime, whereas the equivalent prevalence was 11% in patients diagnosed with bipolar disorder and 3% in controls.
So, I revise my earlier view that there is a fivefold increase in violence in schizophrenia. In this 3 million person population sample, schizophrenics are 7.7 times more violent, bipolars 3.7 times more violent. Some mental disorders lead to violence. It would be good to get more details on the types of violent criminal event, but from the public’s point of view, the picture is clear enough.
http://www.nature.com/mp/journal/vaop/ncurrent/abs/mp2015184a.html
Time to do some further work on detection, and arrange services on the understanding that some prevention of violence is possible, and worth doing.



If schizophrenics are scarcely more of a risk than the general public, then presumably the psychiatrists and jailers in Broadmoor and the like stroll around without taking any special precautions for their safety.
ReplyDeleteAnd if Broadmoor is too demanding a test, surely in any mental hospital nobody bothers with special safety precautions, do they?
You are conflating population statistical risk with individual risk. On the whole offenders are not dangerous, but some are. Same as schizophrenics.
DeleteIncreased risk for a sub-population implies higher risk for members of that sub-population, even when prediction of individual risk is imperfect.
DeleteThanks for this. Discussing these issues with younger psychologist colleagues, I often describe it thus: "If by risk of violence, from a person with mental health problems you mean a 60 year old woman with diagnoses of social phobia and mild depression, then the risk of violence is likely low. If on the other hand you mean a twenty-five year old man, with a diagnosis of paranoid schizophrenia, a history of assault, and who uses alcohol and amphetamines, then living next door to him could be dicey."
ReplyDeleteAn the comorbidity with psychopathy and other disorders*
ReplyDelete